India has a lot to teach America in healthcare: Vijay Govindarajan
ADVERTISEMENT
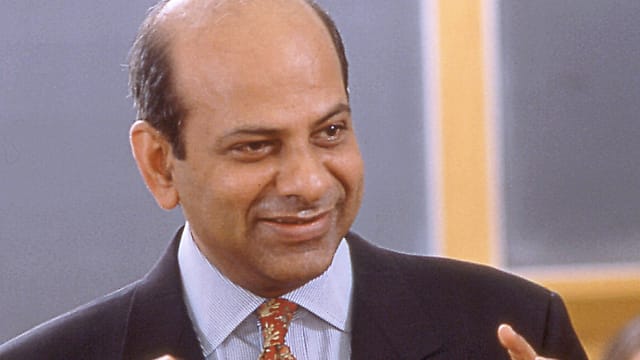
Govindarajan is one of the foremost business thinkers in the world. He is the Coxe Distinguished Professor at Dartmouth College’s Tuck School of Business, and was the Marvin Bower Fellow 2015-16 at Harvard Business School. He is a best-selling author of several books. He talks to Fortune India’s Hindol Sengupta on his new book Reverse Innovation in Healthcare, where he argues that there is much that the developed world can learn from healthcare systems and processes in countries such as India. He has co-authored the book with Ravi Ramamurti, University Distinguished Professor of international business & strategy and director of the Center for Emerging Markets at Northeastern University.
In your book, you distinguish between value-based healthcare instead of delivery-based on volume and fee-for-service. Could you explain the difference between the two?
In the U.S., we have a reimbursement model, fee-for-service, where hospitals are paid for each service they provide to patients. The more X-rays the hospital takes, the higher its revenue. This gives hospitals incentive to provide unnecessary services, which not only creates inefficiencies and drives up costs. This over-treatment of patients can actually decrease medical quality. If a patient stays in the hospital more than is necessary, the patient can potentially catch infections. Suffice it to say, fee-for-service reimbursement incentivises volume of procedures.
Value-base care, on the other hand, is about maximum quality for minimum cost. Under this system, healthcare providers focus on improving patient outcomes, and at the same time, lowering costs. All parties in the health care ecosystem—hospitals, insurance companies, and medical suppliers—put the emphasis on creating value for patients.
We advocate for value-based health care, not volume-based healthcare.
Using this difference, how are the Indian and American models different?
In India, three conditions favour value-based care. The Indian population is huge, poor, and largely uninsured. The Indian healthcare system has a severe shortage of doctors and facilities, and Indian healthcare is not subject to rigorous regulations.
With dramatically fewer doctors, India has to take care of many more patients who can’t afford to pay much (but often still pay out of pocket). Stated differently, the challenge in India is to deliver existing medical knowledge to a large number of patients at an ultralow cost; in short, create breakthrough healthcare delivery innovations. This is what promotes value-based healthcare, where hospitals strive to give quality at low cost. We are not saying that all Indian hospitals provide value-based care. We studied seven Indian hospital exemplars who provide value-based care: Narayana Health, Aravind Eye Care, LV Prasad Eye Institute, Care Hospital, Deccan Hospital, HCG Oncology, and LifeSpring Hospital.
In the U.S., the environment is the opposite of what we find in India. Most Americans are covered by either a government-sponsored insurance scheme or private sector insurance. The patient does not pay for treatment, so they do not care about healthcare costs. Healthcare is a highly regulated industry in the U.S. The U.S. has embraced regulated competition, and not value-based competition. The fee-for-service reimbursement model provides perverse incentives, as we noted above. The country has plenty of medical resources; both doctors and over-built hospital infrastructure. In the U.S., there is little incentive to control healthcare costs, and many incentives to over-utilise healthcare services.
In India, Narayana Health does open heart surgery for $2,000 [approx. Rs 1.34 lakh], whereas the same procedure will cost about $150,000 in the U.S. Yet, Narayana Health’s quality is better than U.S. hospitals. For Narayana Health, mortality rates 30 days after surgery is 1.4%, whereas the U.S. average is 1.9%. That is value-based care! All the other six Indian hospitals have a similar story; world class quality at ultra low cost.
Why do you think the Indian healthcare model is better?
As we noted above, conditions are ripe in India for value-based care. Is it practiced by all hospitals? Definitely not. However, a few exemplar hospitals have embraced five principles to provide world-class quality health care at ultra-low cost:
- Noble purpose: The exemplar hospitals view healthcare as a human right. They serve both rich and poor patients, and provide them with the same quality care. The rich motivate hospitals to keep quality high, and the poor motivate them to keep costs down. The result is a high-quality, low-cost model.
- Hub-and-spoke design: These hospitals use a hub-and-spoke configuration, where the hub hosts the most expensive equipment and high-priced doctors, and spokes house simple equipment and general practitioners. In this model, the hub has high volumes for surgeries that through scale economies, drives down costs and drives up quality.
- Technology: These hospitals are enthusiastic users of technology, including tele-medicine, remote monitoring, home-based care, and electronic medical records. Technology simultaneously improves quality and reduces costs.
- Task shifting: These hospitals over invest in nurses and paramedics to do most of the work with patients and surgeons. Surgeons are scarce and expensive do. Task shifting helps with quality and costs.
- Frugality: Indian hospitals are frugal in both operating costs and capital expenditure. They cut costs to the bone in non-medical areas, but spend as needed on medical care. They avoid unnecessary procedures and train doctors to think about costs by supplying them with financial data.
Some would argue that if India has a good model, why is public healthcare so abysmal here?
The point of our book is not that India is a role model for healthcare delivery, but that a handful of hospitals are role models, because they have found innovative ways to deliver healthcare of high quality at very low cost. Innovation in healthcare delivery by these hospitals has been driven by dire conditions in India, such as the shortage of doctors and the low purchasing power of a large population. If all Indian hospitals emulated the practices of these exemplar hospitals, high-quality healthcare would be much more widely available to the country’s population. It still would not ensure universal access, because the unserved population in India is so vast, but it would move India in that direction.
Take Aravind Eye Care System, for instance. It is at the global frontier of eye care delivery. It is like the Toyota of eye care. It cares for more people each year than the U.K.’s National Health System (NHS), but with only 1-2% of NHS’s budget. Yet, it delivers better quality than the NHS. Aravind is so efficient that the margin it earns on one paying patient is sufficient to treat two non-paying or subsidised patients, and still earn a high return (enough to fund its rapid expansion over the years). Since inception, Aravind has provided eye surgery to more than four million poor people. Hospitals around the world can learn from Aravind’s process innovations. In fact, Aravind has created a special department just to disseminate its best practices to other hospitals. All Indian hospitals, not just eye hospitals, should consider sending teams of doctors and administrators to Aravind to pick up ideas for improving their own operations.
People mistakenly assume that if you lower healthcare costs, you must also lower quality. The Indian exemplars explode this myth. Many of the things they do to improve quality also lowers cost, and many of the things they do to lower cost improve quality. This was the brilliant lesson Toyota taught the world about manufacturing. The Indian exemplars show that the same lesson applies also to healthcare. This is their greatest contribution to the world.
The lessons from the Indian exemplars don’t apply just to not-for-profit hospitals. In fact, five of the seven Indian exemplars we studied are for profit organisations. We hope that for profit Indian hospitals also will consider adopting the five principles mentioned earlier, because they can improve profitability and quality even as they lower costs and prices.
Many of the best Indian hospitals target the well-to-do. Nothing wrong with that. But what these hospitals may be missing is how the poor can contribute to their strategic success. This is a counter-intuitive point and one of the main lessons of our research. It is easy to see the advantages of serving the rich—they can pay high prices, and by demanding high quality, they force the hospital to deliver care at international levels. But serving the poor also has its advantages, even though less obvious. First, the poor contribute volume and help drive down unit costs through economies of scale. Second, they expose doctors to more cases, including relatively rare conditions. The hospital’s doctors become better at their work, because practice makes perfect, and this spills over into care for the rich. Finally, serving the poor motivates the rank-and-file to pursue breakthrough cost innovations in health care delivery, because everyone understands that a penny saved is a penny that can be used to care for another poor patient. Caring for the poor inspires breakthrough innovations. In this way, the rich and poor create value for one another.
How can India improve its public health record and what can it teach America?
Improving India’s public health record involves many challenges—from controlling infectious diseases and promoting healthy lifestyles to expanding medical education, adding hospital beds, and reforming health insurance. Our book focusses on one important slice of this problem—how to deliver quality healthcare to the greatest number, affordably. In the medium term, this is one of the most promising ways to improve healthcare access for the masses. We urge Indian hospitals to embrace the five principles stated earlier.
In the area of healthcare delivery, India has a lot to teach America. America leads the world in medical science, and in the development of new drugs and devices, but it has long ceased to maximise value in healthcare delivery. America spends $10,000 per person annually—more than double any other industrialised country—and yet care is of uneven quality and access is not universal.
In many ways, the U.S. healthcare system practices the opposite of the five principles we identified earlier. For instance, the U.S. has too many high-end, multi-specialty hospitals; that is, too many hubs and not enough spokes. When U.S. hospitals merge, the goal often is to raise prices rather than to streamline operations and evolve into a hub-and-spoke system. Similarly, U.S. healthcare would benefit from a lot more task shifting, so doctors can spend more time caring for patients and less time doing paperwork. (Doctors in top hospitals, like Mayo Clinic, spend half their time on administrative matters.) Even when hospitals are restructured, low-level administrative staff are laid off, making doctors and nurses do more of the paperwork, such as billing and recordkeeping—exactly the wrong kind of task shifting!
U.S. hospitals could also leverage technology much more extensively, for instance, by creating tele-health networks. Insurance companies should agree to reimburse tele-consultations, which are cheaper, timelier, and more convenient for patients. U.S. hospitals could also learn from the Indian exemplars how to be frugal, and stop building hospitals that feel like seven-star hotels but do little to improve medical outcomes. Most of all, leaders of U.S. hospitals need to create a patient-centric organisational culture that motivates employees to find innovative ways to improve quality and lower costs. Everyone in the organisation, including doctors and nurses, must be made to focus on value, as they do in Aravind or Narayana Health.